Introduction
Chiropractic in Guelph for Hip
Welcome to Active Therapeutic Solutions patient resource about Osteoarthritis of the Hip.
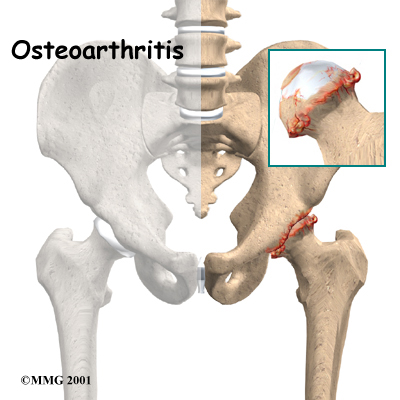
Osteoarthritis (OA) is a common problem for many people after middle age. OA is sometimes referred to as degenerative, or wear-and-tear, arthritis. OA commonly affects the hip joint. In the past, little was done for the condition. Now doctors have many ways to treat hip OA so patients have less pain, better movement, and improved quality of life.
This guide will help you understand:
- how OA develops in the hip
- how doctors diagnose the condition
- what can be done for your pain
#testimonialslist|kind:all|display:slider|orderby:type|filter_utags_names:Hip Pain|limit:15|heading:Hear from some of our patients who we treated for *Hip Pain*#
Anatomy
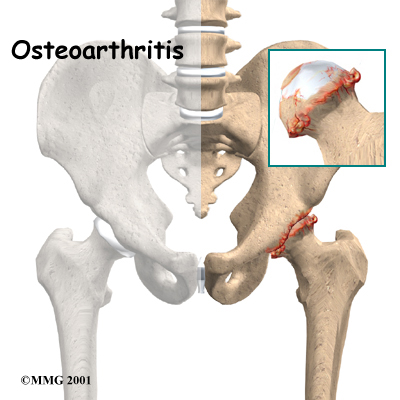
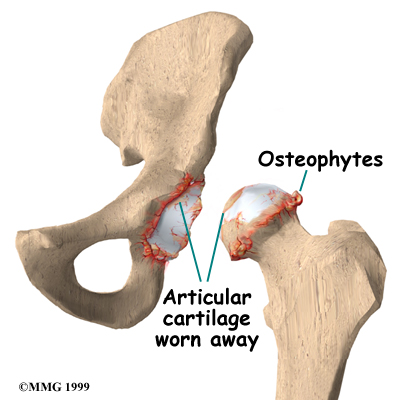
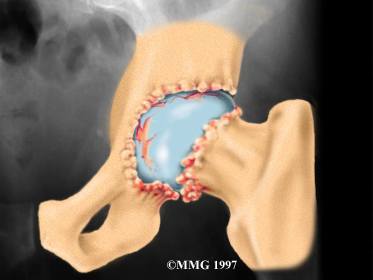
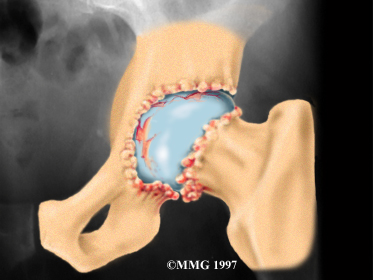
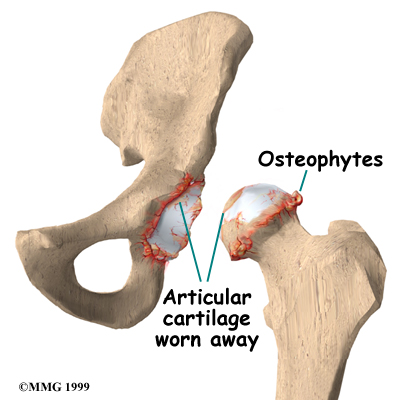
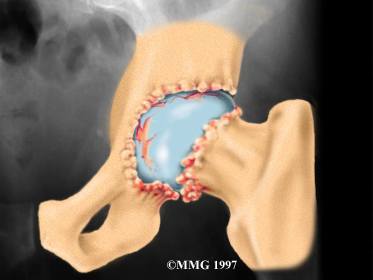
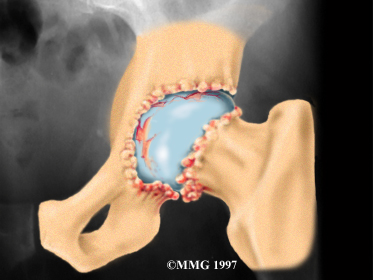
Articular cartilage is the smooth lining that covers the surfaces of the ball-and-socket joint of the hip. The cartilage gives the joint freedom of movement by decreasing friction. The layer of bone just below the articular cartilage is called subchondral bone. The main problem in OA is degeneration of the articular cartilage.
When the , or wears away, the subchondral bone is uncovered and rubs against bone. Small outgrowths called bone spurs or osteophytes may form in the joint.
Related Document: Active Therapeutic Solutionss Guide to Hip Anatomy
Causes
OA of the hip can be caused by a hip injury earlier in life. Changes in the movement and alignment of the hip eventually lead to wear and tear on the joint surfaces. The alignment of the hip can be altered from a fracture in the bones around or inside the hip. If the fracture changes the alignment of the hip, this can lead to excessive wear and tear, just like the out-of-balance tire that wears out too soon on your car. Cartilage injuries, infection, or bleeding within the joint can also damage the joint surface of the hip.
Not all cases of OA are related to alignment problems or a prior injury, however. Scientists believe genetics makes some people prone to developing OA in the hip.
Scientists also believe that problems in the subchondral bone may trigger changes in the articular cartilage. As mentioned, the subchondral bone is the layer of bone just beneath the articular cartilage. Normally, the articular cartilage protects the subchondral bone. But some medical conditions can make the subchondral bone too hard or too soft, changing how the cartilage normally cushions and absorbs shock in the joint.
Avascular necrosis (AVN) is another cause of degeneration of the hip joint. In this condition, the femoral head (the ball portion of the hip) loses a portion of its blood supply and actually dies. This leads to collapse of the femoral head and degeneration of the joint. AVN has been linked to alcoholism, fractures and dislocations of the hip, and long-term cortisone treatment for other diseases.
Related Document: Active Therapeutic Solutions Guide to Avascular Necrosis of the Hip
Symptoms
The symptoms of hip OA usually begin as pain while putting weight on the affected hip. You may limp, which is the body's way of reducing the amount of force that the hip has to deal with. The changes that happen with OA cause the affected hip to feel stiff and tight due to a loss in its range of motion. Bone spurs will usually develop, which can also limit how far the hip can move. Finally, as the condition becomes worse, pain may be present all the time and may even keep you awake at night.
Diagnosis
The diagnosis of hip OA starts with a complete history and physical examination by your doctor. X-rays will be required to determine the extent of the cartilage damage and suggest a possible cause for it.
Other tests may be required if there is reason to believe that other conditions are contributing to the degenerative process. Magnetic resonance imaging (MRI) may be necessary to determine whether your hip condition is from problems with AVN.
Blood tests may be required to rule out systemic arthritis or infection in the hip.
Diagnosis
When you visit Active Therapeutic Solutions, diagnosis of hip OA starts with a complete history and physical examination by one of our therapists.
Some patients may be referred to a doctor for further diagnosis. Once your diagnostic examination is complete, the Chiropractors in Guelph have treatment options that will help speed your recovery, so that you can more quickly return to your active lifestyle.
Our Treatment
Non-surgical Rehabilitation
OA can't be cured, but Chiropractic is available to ease symptoms and to slow down the degeneration of the joint. Nonsurgical rehabilitation of hip OA is used to maximize the health of your hip and to prolong the time before any type of surgery is necessary. Recent information shows that your condition may be maintained and in some cases improved.
Chiropractic plays a critical role in the nonsurgical treatment of hip OA. At Active Therapeutic Solutions, our primary goal is to help you learn how to control symptoms and maximize the health of your hip. Our Chiropractor will recommend ways to calm pain and symptoms, which might include the use of rest, heat, or topical rubs.
We may have you use a cane or walker to ease pressure when walking. Our Chiropractor will use range-of-motion and stretching exercises to improve your hip motion. You will be shown strengthening exercises for the hip to steady the joint and protect it from shock and stress. Our therapist can suggest tips for getting your tasks done with less strain on the joint.
Although the time required for recovery is different for every patient, you will probably progress to a home program within two to four weeks.
In cases of advanced OA where surgery is called for, you may see our Chiropractor before surgery to discuss exercises, special precautions to be followed just after surgery, and to practice walking with crutches or a walker
Post-surgical Rehabilitation
When you begin your Active Therapeutic Solutions post-surgical rehabilitation, our Chiropractor will develop a personalized program of exercises to improve your muscle tone and strength in your hip and thigh muscles and to help prevent the formation of blood clots. Our Chiropractor will also make recommendations about your safety, review special hip precautions and make sure you are placing a safe amount of weight on your foot when standing or walking.
Related Document: Active Therapeutic Solutions Guide to Artificial Hip Dislocation Precautions
A few additional visits to our outpatient Chiropractic facility may be needed for patients who continue having problems walking or who need to get back to physically heavy work or activities.
Our goal is to help you maximize hip strength, restore a normal walking pattern, and do your activities without risking further injury to your hip. When your recovery is well under way, your regular visits to Active Therapeutic Solutions will end. Although we will continue to be a resource, you will be in charge of doing your exercises as part of an ongoing home program.
Active Therapeutic Solutions provides services for Chiropractic in Guelph.
Physican Review
Your doctor will order X-rays to determine the extent of the cartilage damage and suggest a possible cause for it.
Other tests may be required if there is reason to believe that other conditions are contributing to the degenerative process. Magnetic resonance imaging (MRI) may be necessary to determine whether your hip condition is from problems with AVN.
Blood tests may be required to rule out systemic arthritis or infection in the hip.
Your physician may prescribe medicine to help control your pain. Acetaminophen (Tylenol) is a mild pain reliever with few side effects. Some people may also get relief of pain with anti-inflammatory medication, such as ibuprofen and aspirin. Newer anti-inflammatory medicines called COX-2 inhibitors show promising results and seem not to cause as much stomach upset or other intestinal problems. Ensure that you consult with your doctor or pharmacist regarding the use of pain relief or anti-inflammatory medication.
If you aren't able to get your symptoms under control, a cortisone injection may be prescribed. Cortisone is a powerful anti-inflammatory medication, but it has secondary effects that limit its usefulness in the treatment of OA. Multiple injections of cortisone may actually speed up the process of degeneration.
Repeated injections also increase the risk of developing a hip joint infection, called septic arthritis. Any time a joint is entered with a needle, there is the possibility of an infection. Most physicians use cortisone sparingly, and avoid multiple injections unless the joint is already in the end stages of degeneration and the next step is an artificial hip replacement.
Surgery
In some cases, surgical treatment of OA may be appropriate.
Arthroscopy
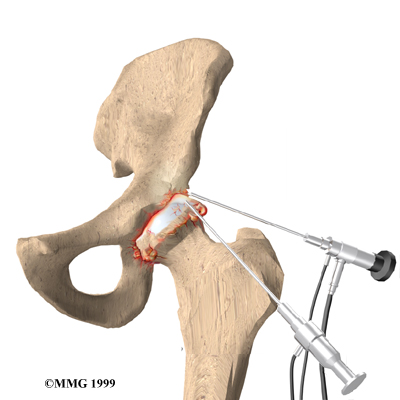
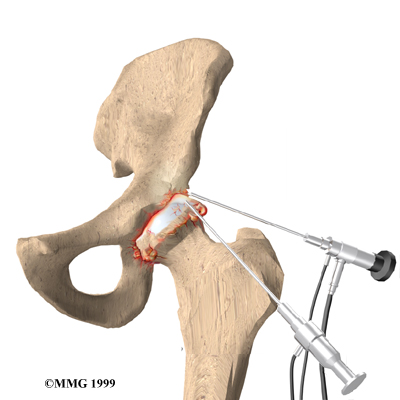
Surgeons can use an arthroscope to check the condition of the articular cartilage in a joint. An arthroscope is a miniature TV camera inserted into the joint though a small incision. While checking the condition of the cartilage, your surgeon may try a few different techniques to give you relief from pain. One method involves cleaning the joint by removing loose fragments of cartilage. Another method involves simply flushing the joint with a saline solution, after which some patients report relief.
This procedure is sometimes helpful for temporary relief of symptoms. Hip arthroscopy is relatively new, and it is unclear at this time which patients will benefit.
Osteotomy
When the alignment of the hip joint is altered from disease or trauma, more pressure than normal is placed on the surfaces of the joint. This extra pressure leads to more pain and faster degeneration of the joint surfaces.
In some cases, surgery to realign the angles of the pelvic socket or femur (thighbone) can result in shifting pressure to the other healthier parts of the hip joint. The goal is to spread the forces over a larger surface in the hip joint. This can help ease pain and delay further degeneration.
The procedure to realign the angles in the joint is called osteotomy. In this procedure, the bone of either the pelvic socket or femur is cut, and the angle of the joint is changed. The procedure is not always successful. Generally it will reduce your pain but not eliminate it altogether. The advantage to this approach is that very active people still have their own hip joint, and once the bone heals, there are fewer restrictions in activity levels.
An osteotomy procedure in the best of circumstances is probably only temporary. It is thought that this operation buys some time before a total hip replacement becomes necessary.
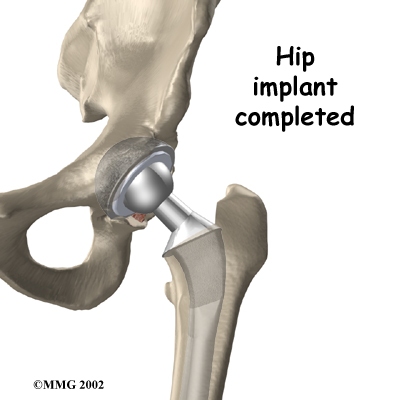
Artificial Hip Replacement
An artificial hip replacement is the ultimate solution for advanced hip OA. Surgeons prefer not to put a new hip joint in patients less than 60 years old. This is because younger patients are generally more active and might put too much stress on the joint, causing it to loosen or even crack. A revision surgery to replace a damaged joint is harder to do, has more possible complications, and is usually less successful than a first-time joint replacement surgery.
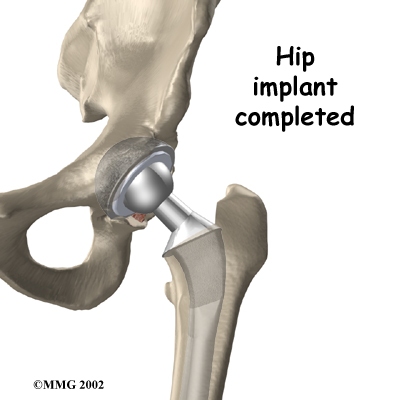
Related Document: Active Therapeutic Solutions Guide to Artificial Joint Replacement of the Hip
Portions of this document copyright MMG, LLC.